
Can stem cell transplants be the way of the future for tackling HIV?

Once is a fluke, twice is a trend! A second reported case of a patient being cured of HIV following a stem cell transplant.
An experimental transplant
Twenty years ago, a German hematologist performed an experiment. Dr. Gero Hütter had a leukemia patient who wasn’t responding to chemotherapy. So he followed the usual procedure and started looking for a bone-marrow donor for a transplant.
But, this wasn’t to be any old transplant. It was to be an experiment that relied on two facts: 1) The patient had HIV and 2) a DNA mutation that made some of us resistant to HIV.
The CCR5 gene
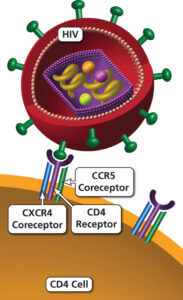
CCR5 acts as a secondary receptor for HIV,
when the virus enters cells
(Image from https://aidsinfo.nih.gov)
Hütter had a read a paper decades ago about a mutation in the CCR5 gene. The gene produces a protein found on the surface of cells (a receptor) that HIV uses to enter immune cells. About 1% of people in Europe inherit two mutated copies of CCR5 and are highly resistant to HIV.
So, the haematologist hypothesized that if he can replace his patient’s bone marrow with donor cells that didn’t have CCR5, he may no longer be susceptible to HIV. And, that is exactly what he did. He was lucky enough to find a possible donor match with the desired mutation.
A single successful experiment
If the transplant holds, the man will be producing immune cells that lacked CCR5 after the transplant. Amazingly, just two years after the procedure, doctors could no longer find signs of HIV in the man, even though he was no longer taking antiretroviral drugs (standard therapy to treat HIV). The experiment appears to have worked!
Unfortunately, the success with the “Berlin patient” wasn’t easily reproduced. That is until recently. There’s a second study that reports similar findings, another leukemia patient who has been HIV free following a bone marrow transplant, suggesting that Berlin patient wasn’t cured just by chance.
Tweaking the experiment
With the recent study, scientists show that aggressive pre-treatment used by Hütter and colleagues to eradicate the patient’s bone marrow is not necessary for a successful stem cell transplant. Both chemotherapy and radiation were used with the Berlin patients. In the new study, only chemotherapy drugs (with reduced side effects compared to radiation) were used.
Hope for the future
 Will stem cell transplants become
Will stem cell transplants become
the way of the future for tacking HIV?
While bone marrow transplants may be a way to tackle HIV in patients with leukemia or other diseases, this treatment option isn’t suitable for HIV patients that don’t need a bone marrow transplant.
However, amazing advances being made in technologies for using stem cells and genetic engineering techniques. This, coupled with more and more parents choosing to bank cord blood and cord tissue samples of their children at birth, a day where a child’s own stem cells can be genetically engineered to treat HIV may not be too far off in the future.
Reference
Gupta, RK, Abdul-Jawed, S, McCoy, LE. et al. (2019) HIV-1 remission following CCR5Δ32/Δ32 haematopoietic stem-cell transplantation. Nature 568, 244–248 (2019). doi: https://doi.org/10.1038/s41586-019-1027-4.
相关文章

Sibling cord blood tested for treating cerebral palsy in young children









