
Non-invasive, intranasal administration of umbilical cord stem cells can restore damage caused by lung disease
Preclinical studies show that umbilical cord stem cells can effectively restore damage from chronic lung disease. This study examines the effectiveness of using a non-invasive delivery method for stem cells, nasal administration, using an experimental model for bronchopulmonary dysplasia.
What is bronchopulmonary dysplasia?
Bronchopulmonary dysplasia (BPD) is a serious lung condition caused by underdeveloped lungs. Affected infants display abnormal changes in the structure or the organization of cells in the smaller airways and the air sacs (alveoli) of the lung, which affects lung function and makes breathing difficult. BPD mostly affects newborn babies who are born prematurely.
Characteristic symptoms of BPD include abnormal developments of blood vessels in the lung, inflammation and compromised repair in the lung. As a result, affected babies are at high risk of developing complications like pneumonia and other infections, leading to frequent hospitalizations. They may also suffer from lifelong heart/lung disease and even experience cognitive deficiencies.
In the US, approximately 12% of all deliveries account for preterm births. It is estimated half of these babies will experience lung problems.
Treating BPD
Newborns with BPD are treated with oxygen therapy, which includes providing oxygen through a mask, nasal prongs or a breathing tube. While oxygen treatment is effective, some babies will continue to experience breathing difficulties into childhood and adulthood.
Because they have fragile lungs affected children are more susceptible to irritants such as smoke and pollutants that can enhance lung damage. Not many treatment options are available for remedying these ongoing symptoms that result from BPD.
Regenerative therapies for BPD
Due to their regenerative potential, stem cells are being explored as a possible treatment option for complex diseases like BPD, where different damaged tissues need to be repaired. Stem cells are early-stage cells that have the capacity to regenerate a number of other cell types.
Mesenchymal stem cells (MSC), in particular, are considered an attractive alternative for regenerative therapies, because they release factors that stimulate the immune system to enhance healing. Several studies have looked at the effectiveness of using MSCs to repair lung injuries in experimental animal models that mimic BPD. However, many of them have focused on providing stem cells intravenously (injecting into a blood vessel) or injecting into the trachea.
A non-invasive way to deliver stem cells
Researchers in this study wanted to develop a less invasive method for introducing stem cells to babies affected with BPD. So they examined whether delivering stem cells using a nasal spray will be as effective as delivering them using the more invasive methods.
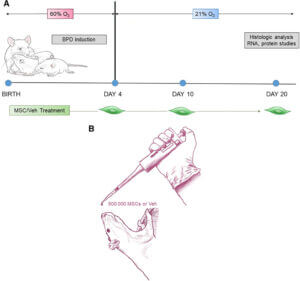 n their experimental model, newborn rats were exposed to low oxygen levels to induce BPD like symptoms. These rats were then treated with intranasal administration of MSCs 4, 10, and 20 days after induction.
n their experimental model, newborn rats were exposed to low oxygen levels to induce BPD like symptoms. These rats were then treated with intranasal administration of MSCs 4, 10, and 20 days after induction.
MSCs used in this study were isolated from the Wharton’s jelly tissue (the gelatinous material inside the umbilical cord) of healthy term human newborns.
They made use of MSCs for the umbilical cord in their study for several reasons. Obtaining umbilical cord stem cells are less invasive than getting adult stem cells.
In the past, the umbilical cord and the cord blood in it used to be discarded as medical waste. But now we know that both cord blood and the cord itself are valuable sources of newborn stem cells.
Intranasal delivery of umbilical cord stem cells restores lung function
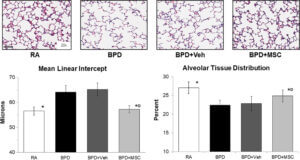 Following treatment, they looked at characteristic signs of BPD to see if the treatment was effective. They found that umbilical cord MSCs were able to restore the damage in both air sacs and blood vessels in the airways.
Following treatment, they looked at characteristic signs of BPD to see if the treatment was effective. They found that umbilical cord MSCs were able to restore the damage in both air sacs and blood vessels in the airways.
For example, rats with BPD like symptoms had fewer and larger sized alveoli, indicating that the development of these structures were affected. But, after treatment, researchers noted improved development of alveoli and alveolar tissue distribution.
They also went on to study further how MSCs induced these regenerative effects and show that it may be through releasing factors that modulate the immune system, support wound healing and promotes the survival of cells.
Non-invasive stem cell delivery for the win
The rationale behind using MSCs was well established before this study. MSCs release factors that promote blood vessel formation and the growth and survival of lung cells. This study highlighted that MSCs can be delivered using a less invasive method via nasal spray. It also showed that umbilical cord stem cells were a good source of stem cells for BPD.
Intranasal administration was viable and was effective and is attractive, mainly because it is non-invasive. Also, it offers the option of administering multiple doses without much discomfort to the patients. Given that patients affected by BPD are newborn infants, this non-invasive method gives a promising new way to offer regenerative therapy to treat them.
Reference:
Moreira, A, Winter, C, Joy, J et al. (2019) Intranasal delivery of human umbilical cord Wharton’s jelly mesenchymal stromal cells restores lung alveolarization and vascularization in experimental bronchopulmonary dysplasia. STEM CELLS Transl Med. 2020;9:221–234. doi: 10.1002/sctm.18-0273.
相关文章

Sibling cord blood tested for treating cerebral palsy in young children









